
Sports Related Injuries of the Foot and Ankle

There are several types of foot and ankle injuries that can occur when playing sports. The most common sports injury is an ankle sprain. It is important for ankle sprains to be diagnosed and treated professionally, as an improperly healed ankle can lead to additional sprains, chronic ankle instability, and arthritis. Another type of injury athletes face involves the Achilles tendon, which can become inflamed, injured, torn, or even ruptured from repetitive activity or trauma. An inflammation of the plantar fascia that runs along the sole of the foot is termed plantar fasciitis. It can be caused by overuse, wearing shoes that are worn out, or footwear that is not appropriate for a particular sport or activity. Running and court sports can lead to a compression of the nerve between the third and fourth toes, resulting in a condition known as Morton’s neuroma. This causes the tissue surrounding the nerve to thicken, and if left untreated may result in nerve damage. If you have suffered a foot, toe, or ankle injury while playing sports, it’s suggested that you contact a podiatrist.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot And Ankle Injuries
Foot and ankle injuries are common among people who participate in sports. Several factors contribute to this. They include failing to stretch or warm up properly, not wearing the proper type of shoe and not taping or providing other types of support for the ankle or foot. The most common foot and ankle injuries suffered by people involved in sports are plantar fasciitis, ankle sprains and Achilles tendon damage or ruptures. If not treated properly, they can lead to permanent disability.
Treating these injuries is relatively simple if they are identified and addressed early. Many athletes dismiss the initial aches and pains associated with injury as just soreness or tired muscles. Their first response is usually to try to work through it. This can lead to serious problems. Many minor injuries are made far more serious when athletes continue to put strain and pressure on them. That attitude can change a mild strain into a serious strain and a minor tear into a rupture. Athletes should have unusual aches and pains evaluated by a skilled medical professional.
Plantar fasciitis is a painful injury. It is inflammation of the plantar fascia, the thick band of tissue running from the heel to the base of the toes. If left untreated, it can lead to a degenerative disease called plantar fasciosis. There are several effective treatments for this ailment. Doctors often prescribe rest, massages, stretching, night splints, physical therapy, anti-inflammatory medication, corticosteroids or surgery, usually in that order. The most effective treatment for plantar fasciitis is orthotics, which offers foot support. Surgery is occasionally used as a last resort, but it comes with the risk of nerve damage and infection and often does not stop the pain.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. Running, jumping and walking all impact this tendon. Two common injuries to the Achilles tendon are tendonitis and a rupture of the tendon. Tendonitis is inflammation in the tendon often caused by an increase in the amount of stress placed on it. Non-surgical treatments include rest, ice or anti-inflammatory medication. A rupture (tear) of the Achilles tendon can be treated by placing the lower leg in a cast for several weeks or with surgery. Many physicians feel surgery is the better option because it lowers the risk of re-ruptures. Both methods require 4 to 6 months of rehabilitation.
Ankle sprains are the most common sports related foot and ankle injury. A sprain occurs when the ligament holding the ankle bones and joint stretches beyond its normal range. It can be treated non-surgically with a combination of rest, ice wrapped around the joint for 30 minutes immediately after injury, compression by a bandage and elevating the ankle above the heart for 48 hours. This combination is referred to as RICE. Severe ankle sprains in which the ligaments are torn may require reconstructive surgery followed by rehabilitation.
Causes and Treatment of Corns on the Feet

Corns on the feet can stem from various factors, with age being one of them. As people grow older, their feet undergo physical and biomechanical changes. These can affect how they function and alter the way you walk, potentially leading to corns. WearingiIll-fitting socks can also contribute to corns on the feet. Too large socks may slip and cause friction, while tight socks can irritate the skin. Shoes that do not fit properly, especially high-heeled or narrow shoes, whether too big or too small, can cause friction and pressure, causing a corn to develop. Obesity can alter your gait and weight distribution, often resulting in foot deformities like flat feet, which in turn make corns more likely to develop. Hammertoes or bunions exert unusual pressure on parts of the foot, promoting corn formation. A podiatrist can treat a foot corn by trimming the skin with a sharp tool to remove the outer layers of the corn. Another option is corn reduction, which calls for cutting away excess bone, repositioning larger bones, or attaching joints. In some cases, a cortisone injection directly into the corn can provide significant relief. If you are suffering from the pain of corns on the feet, it is suggested that you schedule an appointment with a podiatrist.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Corns
Corns are hard and thick areas of skin that form as a result of constant rubbing, friction, or pressure on the skin. They are patches of dead skin with a small plug toward the center. They may appear on the tops and sides of toes and can make walking painful.
Soft corns are typically thinner with a white color and rubbery texture. Soft corns tend to appear between the toes. Seed corns are another type of corn that appear in clusters and can be tender if they are on a weight-bearing part of the foot. Seed corns usually appear on the bottom of the foot and are likely caused by a blockage in sweat ducts.
While corns and calluses are somewhat similar, calluses are a bit different. Calluses are a patch of dead skin that can occur anywhere on the body. In comparison to corns, calluses are usually a bit larger in size. However, both corns and calluses are caused by increased friction on the skin.
There are some risk factors that may increase your chances of developing corns and calluses. If you have bunions, hammertoe, or a bone spur, you are more likely to develop a corn or callus on your foot.
While Corns and Calluses tend to disappear when the friction to the affected area ceases, the help of a podiatrist may be useful in the removal process. It is important to remove the dead skin around the area and this may be done in a few different ways. Moisturizing creams may be helpful in softening and removing the dead skin around the callus. You should never use razors or other pedicure equipment to remove your corns. Doing this may worsen your corn or callus and cause infection.
In some cases, corns and calluses may be caused by abnormal foot structure or walking motion. In such a case, you should seek a podiatrist’s assistance in order to correct the issue.
Wounds That Don't Heal Need to Be Checked
Improving Poor Foot Circulation

Poor foot circulation can lead to discomfort and potentially serious health issues. To improve foot circulation, start by incorporating regular physical activity into your routine, such as walking or swimming, to stimulate blood flow. Elevating your feet when sitting or lying down can also help to reduce swelling and promote circulation. Avoid crossing your legs for long periods, as this can restrict blood flow. Massage therapy can be beneficial for increasing circulation and reducing muscle tension. Wearing compression socks or stockings can improve circulation by helping veins and muscles move blood more effectively. Staying hydrated and maintaining a balanced diet can help to support overall vascular health. Lastly, quitting smoking and managing conditions like diabetes and high blood pressure can further improve blood flow to the feet. If you have poor foot circulation, it is suggested that you contact a podiatrist who can help you manage this condition by guiding you toward additional effective relief strategies.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
Painful Flat Feet
 Flat feet, or pes planus, is a condition where the arches of the feet collapse, causing the entire sole to make contact with the ground. While some individuals with flat feet experience no symptoms, others may face a range of issues. Included are foot pain, overpronation, and discomfort in the ankles, knees, hips, and lower back due to improper alignment and weight distribution. Flat feet can lead to fatigue and difficulty in standing or walking for extended periods. To manage flat feet, wearing supportive shoes with strong arch support and cushioning is essential. Custom orthotics can provide personalized support, alleviating pressure and improving alignment. Regular stretching and strengthening exercises for the feet and calves can enhance flexibility and stability. If you have painful flat feet and discomfort persists, it is suggested that you consult a podiatrist.
Flat feet, or pes planus, is a condition where the arches of the feet collapse, causing the entire sole to make contact with the ground. While some individuals with flat feet experience no symptoms, others may face a range of issues. Included are foot pain, overpronation, and discomfort in the ankles, knees, hips, and lower back due to improper alignment and weight distribution. Flat feet can lead to fatigue and difficulty in standing or walking for extended periods. To manage flat feet, wearing supportive shoes with strong arch support and cushioning is essential. Custom orthotics can provide personalized support, alleviating pressure and improving alignment. Regular stretching and strengthening exercises for the feet and calves can enhance flexibility and stability. If you have painful flat feet and discomfort persists, it is suggested that you consult a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Randy Garr from Bigfoot Podiatry. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a condition that occurs when the arches on the foot are flattened, which allows the soles of the feet to touch the floor. Flatfoot is a common condition and it is usually painless.
Throughout childhood, most people begin to develop arches in their feet, however, some do not. Those who do not develop arches are left with flatfoot. The pain associated with flat feet is usually at its worse when engaging in activity. Another symptom that may occur with those who have this condition is swelling along the inside of the ankle.
It is also possible to have flexible flatfoot. Flexible flatfoot occurs when the arch is visible while sitting or standing on the tiptoes, but it disappears when standing. People who have flexible flatfoot are often children and most outgrow it without any problems.
There are some risk factors that may make you more likely to develop flatfoot. Those who have diabetes and rheumatoid arthritis have an increased risk of flatfoot development. Other factors include aging and obesity.
Diagnosis for flat feet is usually done by a series of tests by your podiatrist. Your podiatrist will typically try an x-ray, CT scan, ultrasound, or MRI on the feet. Treatment is usually not necessary for flat foot unless it causes pain. However, therapy is often used for those who experience pain in their flat feet. Some other suggested treatment options are arch supports, stretching exercises, and supportive shoes.
What Is Morton’s Neuroma?
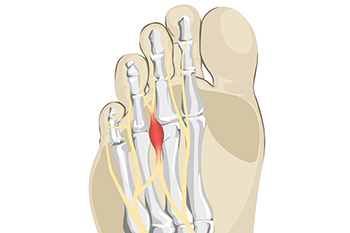
One common cause of foot pain is Morton’s neuroma, a thickening of the nerve tissue between the toes. This condition usually affects the space between the third and fourth toes, causing symptoms such as burning pain, tingling, numbness, and a strange sensation like walking on a pebble. Pain is often worsened by wearing shoes that are too tight or have high heels. Morton’s neuroma can be diagnosed through medical history and physical examination. In some cases, imaging studies may be needed to rule out other causes of foot pain. Treatment often includes resting the foot, wearing orthotics, and taking medications to reduce pain. In many cases, surgical intervention is needed. If you have symptoms of Morton’s neuroma, it is suggested you make an appointment with a podiatrist for care and treatment options.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.