
Sesamoiditis and Foot Pads
Sesamoiditis is a particular kind of foot affliction in which the two small sesamoid bones located in the ball of the feet become inflamed and aggravated. Sometimes, individuals living with sesamoiditis may experience some kind of pain due to their condition. If the individual is prone to engage in activity that puts a significant amount of pressure on the balls of the feet, then pain from sesamoiditis is even more likely. Patients with sesamoiditis will often wonder how they can mitigate the pain caused by the condition. One potential option is to wear sesamoiditis insoles that are like pads for the feet. Some of these foot pads wrap around and support the ball of the foot. These insoles are useful because they can absorb shock in such a way that lessens the pain caused by sesamoiditis. Additionally, these pads can be helpful because they sometimes fit comfortably in the shoes one wears. If you have sesamoiditis, contact a podiatrist today to discuss the possibility of foot pads.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
Foot Blisters and Children

Blisters are certain areas of the skin that can be covered by a bubble-like substance, filled with some kind of bodily fluid. Blisters can often cause an individual a considerable amount of discomfort. Blisters are also generally unsightly. It is important to note that children can develop blisters on their feet for many different reasons. Notably, blisters can result from hand, foot, and mouth disease. As a result of this disease, children typically develop spots on their feet and hands. These spots can then lead to blisters. Parents should be aware of the fact that the fluid in the blisters, if spread, can also transmit the disease. Therefore, if your child has hand, foot, and mouth disease, you should be especially mindful of any blisters that may develop. Contact a podiatrist today if you have concerns about this disease.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
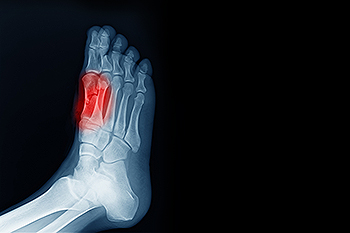
Signs of Peripheral Artery Disease
Peripheral artery disease, PAD, is a circulatory condition that affects the lower limbs and feet, among other extremities. It is the result of a buildup of fat and plaque in the artery walls that restricts blood flow. Signs that you may have peripheral artery disease include pain, numbness, and a feeling of coldness. In addition, if you have PAD, you may notice that minor wounds on the ankle or foot take an unusually long time to heal. You may be more at risk of having PAD if you are a diabetic, have high blood pressure or high cholesterol, and if you are a smoker. If left untreated, PAD can cause serious health problems, including gangrene and, in extreme cases, the loss of a limb. A podiatrist can examine your feet and ankles to determine if peripheral artery disease is the cause of your symptoms. Tests may include checking the pulse in the feet, as well as taking CT or ultrasound scans. For more information about peripheral artery disease in the feet, please contact a podiatrist.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Randy Garr from Bigfoot Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Are Bunions Affecting Your Everyday Life?
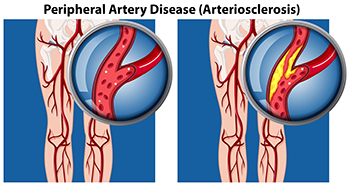
Morton’s Neuroma Surgery
Sometimes, certain afflictions of the foot can be so severe that they can only be treated properly by undergoing a kind of surgical procedure. It is important to note that foot surgery is not for everyone and you may not be a good candidate for particular surgical procedures. However, sometimes undergoing a surgical procedure can be beneficial and it might be the only way to treat severe conditions. For example, some individuals can benefit from a surgical procedure for Morton’s neuroma. This condition is defined as the swelling or inflammation of the nerve between the toes or metatarsal bones. The surgical procedure to address Morton’s neuroma consists of removing a small section of the nerve. An incision must be made to get to the damaged nerve and then the skin is quickly sewn up following the removal of the nerve. Contact a podiatrist today for more information about Morton’s neuroma or to learn if you might be a good candidate for surgery.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Dr. Randy Garr of Bigfoot Podiatry. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.
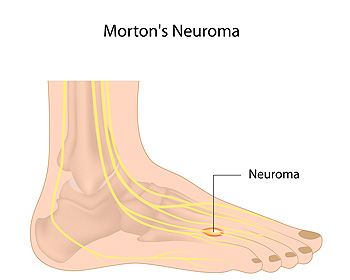
Broken Toe and Nerve Injury

When an individual breaks their toe, the fracture might cause any number of different side effects in relation to the toe. For example, one important side effect of breaking your toe includes, in some cases, the possibility of nerve damage. There are several significant nerves in the toes. In fact, there is a nerve on each side of each toe. Not only does this mean that the toes can be particularly sensitive, it also means that a broken toe can cause nerve damage. It is important to note that if you develop sensations of numbness in the toe after a fracture occurs, then you should seek out medical attention immediately, as this is a sign of nerve damage. Those who suffer from diabetes are at an increased risk of experiencing some kind of nerve damage or abnormality. If you have recently endured a toe fracture and are concerned about the ramifications that it might have on the nerves in your feet, consult a podiatrist today.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Dr. Randy Garr from Bigfoot Podiatry. Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our office located in Provo, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.











